- How to Handle Complex Patient Scenarios in Written Assignments
Nursing education challenges BSN Class Help students with complex patient scenarios in written assignments to simulate real-life clinical decision-making. These assignments not only test your knowledge of anatomy, physiology, pathophysiology, pharmacology, and nursing interventions but also evaluate your ability to critically think, prioritize, and communicate effectively in writing.
Handling complex patient scenarios in written form can be daunting. It requires a structured approach, critical analysis, and a thorough understanding of clinical concepts. This article offers practical guidance on how to effectively manage these intricate case studies, ensuring that your assignments are clear, comprehensive, and demonstrate clinical competence.
Understanding Complex Patient Scenarios
Complex patient scenarios often depict patients with multiple, interrelated health problems, sometimes compounded by psychosocial or ethical issues. They challenge you to:
- Integrate theory and practice.
- Identify priority problems.
- Plan appropriate nursing interventions.
- Anticipate potential complications.
- Reflect on holistic care, including psychosocial and cultural aspects.
The key to success lies in breaking down the complexity into manageable parts and applying a systematic approach.
Step 1: Carefully Analyze the Scenario
Before beginning your assignment, read the patient scenario multiple times. Take notes and highlight key information:
- Patient demographics: Age, gender, background.
- Presenting complaint: Symptoms, duration, severity.
- Medical history: Chronic conditions, surgeries, allergies.
- Current medications: Dosage, frequency, purpose.
- Vital signs and lab results: Indicators of patient status.
- Psychosocial context: Family, cultural factors, emotional state.
- Nursing observations: Behavior, pain levels, mobility.
This thorough analysis sets the foundation for accurate assessment and planning.
Tips:
- Create a timeline if the scenario involves progression or changes.
- Use tables or charts to organize data if allowed.
- Clarify any terms or medications you are unfamiliar with through research.
Step 2: Identify Nursing Diagnoses or Problems
Based on your assessment, determine the nursing diagnoses or main problems. Use standardized nursing language, such as NANDA-I, to articulate these clearly.
- Prioritize issues by severity and urgency.
- Distinguish between actual problems (e.g., impaired gas exchange) and potential risks (e.g., risk for infection).
- Include psychosocial or emotional concerns if relevant.
For example, if a patient has pneumonia and diabetes, nursing diagnoses may include impaired respiratory function and risk for unstable blood glucose levels.
Step 3: Set Measurable and Realistic Goals
For each nursing diagnosis, establish specific goals or expected outcomes. Goals should be:
- Patient-centered: Focus on what the patient will achieve.
- Measurable: Define how success will be evaluated.
- Realistic: Ensure the goals are achievable given the patient’s condition.
- Time-bound: Specify a timeframe, e.g., within 24 hours or by discharge.
For instance, a goal for impaired mobility might be: "Patient will ambulate 20 feet with assistance within 48 hours."
Step 4: Develop Evidence-Based Nursing Interventions
Interventions are the actions you plan to address the patient’s problems and achieve the goals. These should be:
- Specific and detailed: Explain what you will do, how, and why.
- Evidence-based: Support interventions with current nursing research or clinical guidelines.
- Holistic: Address physical, emotional, social, and cultural needs.
- Collaborative: Include referrals to other healthcare professionals when necessary.
Examples of interventions for a patient nurs fpx 4025 assessment 2 with congestive heart failure may include monitoring fluid intake/output, educating on low-sodium diet, and administering prescribed diuretics.
Step 5: Rationalize Each Intervention
A critical part of written assignments is explaining the rationale behind each nursing action. This shows you understand the clinical reasoning process.
- Link interventions to pathophysiology, patient safety, or symptom relief.
- Use citations from credible sources such as nursing textbooks or peer-reviewed articles.
- Avoid vague statements; be specific about how the intervention benefits the patient.
Example: "Administering oxygen therapy helps increase oxygen saturation, alleviating hypoxia caused by impaired gas exchange (Smith, 2020)."
Step 6: Anticipate Complications and Plan Preventative Actions
Complex patient scenarios often carry risks for complications. Identify potential issues and outline how to prevent or manage them.
- Think about the patient’s vulnerabilities based on their condition.
- Include monitoring parameters to detect early signs of complications.
- Address patient education to promote self-care and adherence.
For example, a patient on anticoagulants may be at risk for bleeding; therefore, monitor for signs of hemorrhage and educate on avoiding injury.
Step 7: Incorporate Patient Education and Psychosocial Support
Nursing care is holistic. Reflect on how you will educate and support the patient and their family.
- Explain the condition and treatments in understandable language.
- Discuss lifestyle modifications, medication adherence, and symptom monitoring.
- Consider emotional, cultural, and spiritual needs.
- Include referrals to social workers, counselors, or support groups if relevant.
Patient education improves outcomes and fosters empowerment.
Step 8: Write Clearly and Organize Your Assignment Effectively
Your written submission should be coherent, logical, and well-structured.
- Use headings and subheadings (e.g., Assessment, Nursing Diagnoses, Goals, Interventions).
- Write in formal academic style, avoiding slang or contractions.
- Use active voice and concise sentences.
- Proofread to eliminate errors in grammar, spelling, and punctuation.
Many instructors use rubrics that reward clarity and organization, so pay attention to formatting requirements.
Step 9: Cite Your Sources Properly
Always back up your clinical decisions and explanations with references.
- Use the required citation style (commonly APA for nursing).
- Cite textbooks, journal articles, clinical guidelines, or reputable websites.
- Avoid excessive quoting; paraphrase in your own words.
Proper referencing demonstrates academic integrity and critical appraisal skills.
Step 10: Reflect on the Scenario
If the assignment allows, include a reflection on what you learned or found challenging.
- Consider how the scenario relates to real-world nursing.
- Reflect on how you would improve your clinical skills.
- Discuss the importance of interprofessional collaboration.
Reflection deepens your learning and helps you internalize nursing concepts.
Common Challenges and How to Overcome Them
Challenge 1: Overwhelming Amount of Information
Complex cases can feel like data overload.
Solution: Organize information systematically, prioritize key problems, and focus on relevant details.
Challenge 2: Difficulty Prioritizing Care
Knowing which problem to address first is critical.
Solution: Use frameworks like Maslow’s hierarchy of needs or ABCs (Airway, Breathing, Circulation) to rank priorities.
Challenge 3: Writing Clearly Under Time Constraints
Complex assignments often have tight deadlines.
Solution: Plan your work in stages—assessment, planning, writing, revising—to avoid last-minute stress.
Challenge 4: Integrating Evidence Without Overloading the Paper
Balancing your voice with citations is tricky.
Solution: Summarize evidence succinctly and relate it directly to your interventions and rationale.
Practical Example: Applying the Steps
Let’s consider a simplified example to illustrate these steps:
Scenario: A 65-year-old male with chronic obstructive pulmonary disease (COPD) admitted with exacerbation. He has a history of smoking, shortness of breath, productive cough, and is on inhalers and steroids.
Step 1: Analyze
- Age: 65
- Presenting complaint: Increased shortness of breath, cough with sputum
- History: COPD, smoker for 40 years
- Medications: Bronchodilators, steroids
- Vitals: Increased respiratory rate, low oxygen saturation
- Psychosocial: Lives alone, anxious about hospitalization
Step 2: Nursing Diagnoses
- Impaired gas exchange related to airway inflammation and mucus production.
- Anxiety related to breathlessness and hospitalization.
Step 3: Goals
- Patient will maintain oxygen saturation 92% within 24 hours.
- Patient will demonstrate reduced anxiety as evidenced by calm behavior and verbalization.
Step 4: Interventions
- Administer oxygen therapy as ordered to improve oxygenation.
- Assist with breathing exercises to enhance lung expansion.
- Provide education about inhaler use and smoking cessation.
- Offer emotional support and involve family if possible.
Step 5: Rationales
- Oxygen therapy corrects hypoxemia and reduces respiratory distress.
- Breathing exercises improve ventilation and sputum clearance.
- Proper inhaler use optimizes medication delivery and efficacy.
- Emotional support decreases anxiety, which can worsen dyspnea.
Step 6: Complications
- Monitor for respiratory failure signs.
- Educate on avoiding respiratory irritants.
Step 7: Patient Education
- Teach smoking cessation strategies.
- Discuss medication adherence.
Final Tips for Excellence
- Practice writing patient scenarios regularly.
- Seek feedback from instructors or peers.
- Use clinical guidelines and nursing handbooks.
- Join study groups for discussion and peer support.
- Stay updated with current nursing research.
Conclusion
Handling complex patient nurs fpx 4005 assessment 4 scenarios in written assignments is an essential skill in nursing education, blending clinical knowledge with critical thinking and communication. By methodically analyzing the scenario, prioritizing problems, planning evidence-based interventions, and writing clearly and professionally, you can create assignments that not only earn high grades but prepare you for competent and compassionate nursing care.
Approach each case with curiosity, thoroughness, and respect for the patient as a whole person. With practice and dedication, you will master this important academic and professional skill.
- Integrate theory and practice.
Vyhľadávanie
populárne príspevky
-
 12 najkrajších vianočných rozprávok a komédií, ktoré by ste si s deťmi mali pozrieť
Autor: Martin Zich
12 najkrajších vianočných rozprávok a komédií, ktoré by ste si s deťmi mali pozrieť
Autor: Martin Zich -
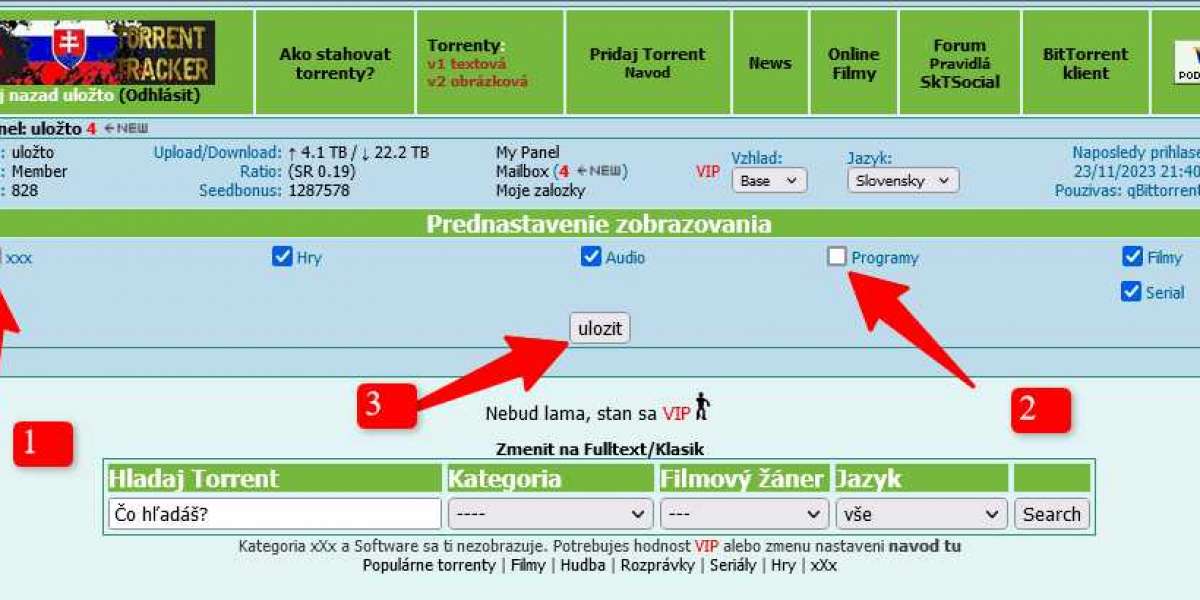 Nastavenie kategorii zobrazovania (zapnutie XXX a Software)
Autor: Martin Zich
Nastavenie kategorii zobrazovania (zapnutie XXX a Software)
Autor: Martin Zich -
 Community Hobbies in Dubai Meetups for Every Interest and Passion
Autor: jukulim lao
Community Hobbies in Dubai Meetups for Every Interest and Passion
Autor: jukulim lao -
 Strážci Galaxie celá filmová séria v jednom blogu (2014-2023)
Autor: Martin Zich
Strážci Galaxie celá filmová séria v jednom blogu (2014-2023)
Autor: Martin Zich -
 gates of olympus game
Autor: sasafarben
gates of olympus game
Autor: sasafarben